Elopement in Borderline Personality Disorder (BPD): Understanding the Role of the Amygdala
Elopement, or wandering behavior, is often associated with autism spectrum disorder (ASD), but it can also be a concern in Borderline Personality Disorder (BPD). In BPD, elopement-like behaviors are driven by intense emotional responses and the need to escape overwhelming situations. Understanding the amygdala’s role in these behaviors provides insight into the emotional dysregulation characteristic of BPD.
The Amygdala in BPD
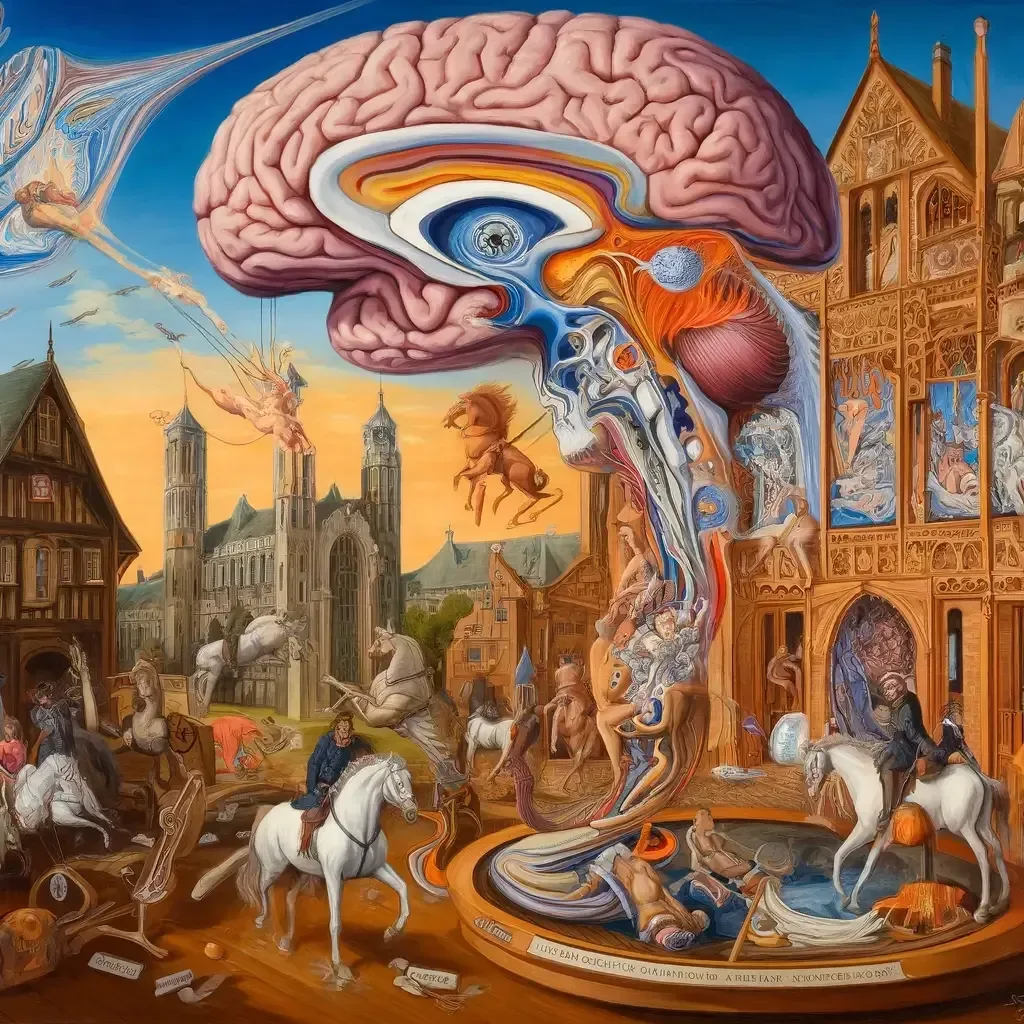
The amygdala is a small, almond-shaped structure deep within the brain that plays a crucial role in processing emotions, particularly fear and pleasure. It is involved in triggering the fight-or-flight response when faced with perceived threats. In individuals with BPD, the amygdala tends to be hyperactive, leading to heightened emotional responses.
- Emotional Dysregulation:
- The hyperactivity of the amygdala in BPD results in intense and often rapid shifts in emotions. This heightened sensitivity can cause impulsive behaviors, including the sudden urge to flee from distressing situations.
- Stress Response:
- The amygdala’s role in the fight-or-flight response means that individuals with BPD may experience intense fear and anxiety in stressful situations, prompting them to escape as a form of immediate relief.
- Fear of Abandonment:
- A key feature of BPD is an intense fear of abandonment. The amygdala’s heightened sensitivity to social cues can amplify this fear, leading to elopement-like behaviors as individuals attempt to avoid perceived rejection or abandonment.
- Impaired Theory of Mind:
- Individuals with BPD may also struggle with theory of mind, particularly in accurately interpreting others’ intentions and emotions. This can lead to misunderstandings and heightened emotional responses, further contributing to the impulse to elope from distressing social interactions.
The Amygdala in Autism Spectrum Disorder (ASD)
In contrast, the amygdala also plays a significant role in autism spectrum disorder, but the nature of its involvement differs from that in BPD.
- Structural Differences:
- In autistic individuals, the amygdala may show atypical development. Studies often find early overgrowth of the amygdala in young autistic children, followed by a period of arrested growth or volume reduction in adolescence or adulthood.
- Heightened Sensitivity:
- The amygdala in autism is often associated with heightened sensitivity to sensory inputs and social stimuli. This can lead to increased anxiety and fear responses, particularly in unfamiliar or overwhelming environments.
- Fight-or-Flight Response:
- Similar to BPD, the amygdala in autism triggers the fight-or-flight response. However, in autism, this response is frequently due to sensory overload or difficulties with social interactions, leading to behaviors such as elopement as a means of seeking safety.
Comparing the Amygdala in BPD and Autism
While both BPD and autism involve the amygdala in heightened emotional responses, the underlying mechanisms and manifestations differ.
- Emotional Dysregulation vs. Sensory Sensitivity:
- In BPD, the amygdala’s hyperactivity leads to emotional dysregulation and impulsivity, often driven by interpersonal conflicts and fears of abandonment.
- In autism, the amygdala’s response is more related to sensory sensitivity and social anxiety, leading to behaviors aimed at escaping overwhelming sensory or social environments.
- Triggers for Elopement:
- BPD-related elopement is often triggered by intense emotional responses to relational stressors.
- Autism-related elopement is typically triggered by sensory overload or fear in unfamiliar situations.
Social Impairments in Autism
One key difference between autism and BPD is the nature of social impairments.
- Social Communication:
- Autistic individuals often struggle with social communication, including understanding and responding to social cues. This can lead to misunderstandings and increased social anxiety.
- Theory of Mind:
- Many autistic individuals have difficulties with theory of mind, or the ability to understand others’ perspectives. This can make social interactions challenging and contribute to the anxiety that triggers elopement.
- Routine and Predictability:
- Autistic individuals often rely on routine and predictability to feel safe. Disruptions to their routine can cause significant distress, leading to behaviors like elopement as they seek to regain a sense of control and safety.
Conclusion
While elopement can occur in both BPD and autism, the underlying causes and manifestations differ significantly due to the distinct roles of the amygdala in each condition. Understanding these differences is crucial for developing effective support strategies tailored to the unique needs of individuals with BPD and autism. By recognizing the specific triggers and responses associated with each disorder, caregivers and professionals can better manage and prevent elopement, ensuring the safety and well-being of those affected.